What is Plantar Fasciitis?
What is Plantar Fasciitis?
Heel pain affects about 10% of adults at any given time. It is estimated that 80% of heel pain is caused by a condition known as “plantar fasciitis”. Here are the basics you need to know if you suspect you might have this condition.
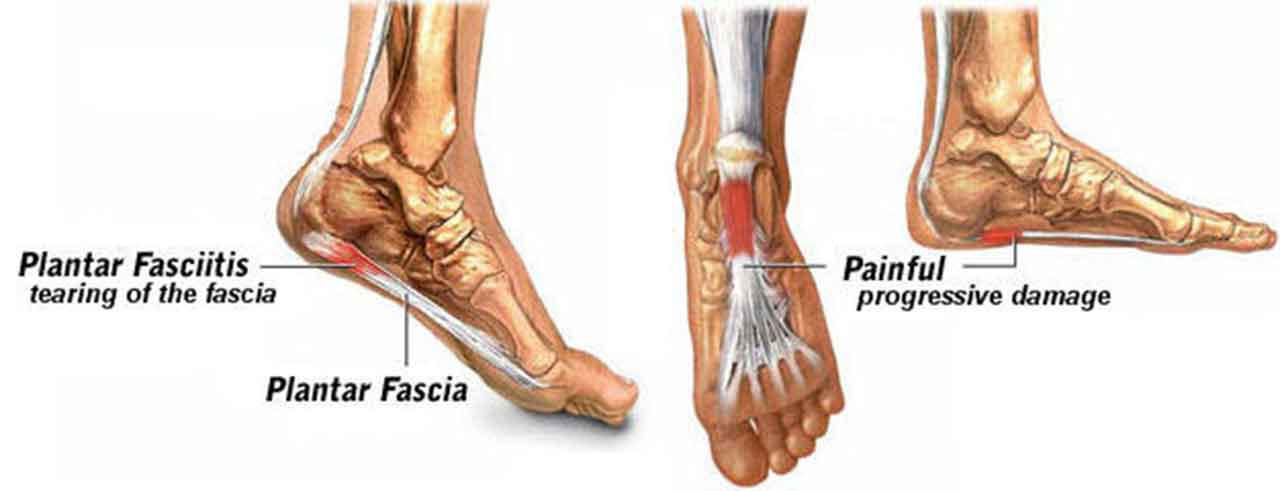
Plantar fasciitis is an inflammation of the plantar fascia.
“Plantar” means “bottom”; so it indicates the bottom of the foot.
“Fascia” is a band of fibrous connective tissue enveloping, separating, or binding together muscles, organs, and other soft structures of your body. The plantar fascia is similar to a ligament, which connects your heel bone to the base of your toes.
Plantar fasciitis usually causes intense pain on the bottom of your foot where your arch meets your heel, especially during the first few steps after getting out of bed in the morning.
Small repetitive injuries to the plantar fascia that occur at a rate faster than the body can heal them cause the pain you feel.
It often goes away once you start to walk around, returning after sitting for some time, or in the early evening.
Plantar Fasciosis: When Fasciitis Becomes Chronic
Plantar fasciosis is a degeneration (this chronic form is no longer an inflammation) of the fascia band.
Plantar fasciosis happens after plantar fasciitis has gone on too long without resolution. At this point, permanent changes to your foot may begin.
Treatment for plantar fasciosis is more difficult, and in some cases, may never resolve completely.
What Causes Plantar Fasciitis?
This condition can be caused by
- extensive running/walking,
- standing for long periods of time, especially on hard surfaces,
- a sedentary lifestyle,
- poor shoe support,
- being overweight,
- overuse,
- sudden stretching of the bottom of your foot,
- a tight Achilles tendon,
- increasing age, which decreases plantar fascia flexibility and thins the heel’s protective fat pad,
- diabetes.
Do I Have Plantar Fasciitis?
Plantar fasciitis has no visible signs. You’ll most often have a deep, localized, painful spot in or around the middle of the sole of the heel or just where your arch and heel meet. It is usually worse on standing after long periods of rest, particularly first thing in the morning.
Plantar fasciitis usually occurs in one foot at a time. Although having it in both feet at the same time is possible, the problem is likely to be something other than plantar fasciitis.
Heel Spurs
Plantar fasciitis is occasionally called a “heel spur”. It isn’t, but sometimes you’ll have one that shows up on an x-ray. Although the name implies a piece of bone sticking out of the heel bone (heel spur syndrome), most people with heel spurs have no pain at all.
Plantar fasciitis is not caused by “heel spurs”.
You don’t need to have surgery to remove a heel spur in order to fix plantar fasciitis.
Plantar Fasciitis Treatment
Minor, acute (having pain for less than a couple of months) plantar fasciitis will often respond to self-care if you are committed to it. This assumes that you actually have plantar fasciitis in the first place.
If self-care doesn’t significantly reduce your plantar fasciitis pain in 2 weeks, it is not likely to do so if you keep doing it. The risk in continuing ineffective self-care is that you can cause a chronic condition where you otherwise wouldn’t.
If self-care isn’t working, please come see me; you either don’t have plantar fasciitis, or you need care only available from a doctor.
What Doctors Do to Treat Plantar Fasciitis
Physical therapy, taping/strapping, orthotics, injections, and medication are commonly used by physicians to heal plantar fasciitis, although no treatment should be cookie-cutter.
In some cases ESWT (Extracorporeal shockwave therapy) can be very effective. It uses sound waves to help heal plantar fasciitis, among other injuries and conditions.
Everyone’s feet are different, so any doctor you see should do what’s right for you, not just a “one-size fits all” management of your condition.
Will you need surgery? Not likely! Less than 2% of plantar fasciitis cases I see require surgery and is always a last resort.
About Self-Taping / Strapping for Plantar Fasciitis
Taping the sole of your foot (also called strapping) can alter the direction of plantar fascia’s stretch and help alleviate symptoms in the short-term.
In the course of someone’s search to learn about plantar fasciitis online, they often find instructions how to tape their own foot. It looks easy to do. The occasional patient successfully does so.
However, the majority of people who try self-taping to relieve plantar fasciitis pain fail to do so correctly. This can sometimes even increase their pain and can create further damage to the fascia.
And, of course, tape loosens and falls off when your feet sweat, so it needs frequent re-application.
I’m not writing this in an effort to scare you into seeing a doctor. Truly, self-taping correctly isn’t as easy as it looks, and often fails to give you the relief you seek.
Try it if you must, at your own risk.
Physician Taping and Use of Orthotics to Cure Plantar Fasciitis
I do find that correctly applied taping and padding can help alter your foot’s biomechanics sufficiently to allow for acute pain relief. This taping/strapping is done with the explicit intention of correctly altering your biomechanics, not just to give you some arch support.
Arch support can be helpful in the short term but does not do the same thing as taping/strapping.
Arch supports will provide pain relief, but won’t fix the actual reason you have plantar fasciitis. If the underlying reason for your plantar fasciitis isn’t fixed, it is more likely to come back. Once that happens a few times, the situation can become chronic (plantar fasciosis) and may be very difficult to completely resolve.
So, physician taping/strapping can prevent that downward spiral into a chronic condition while relieving pain, and tells us if we’re on the right track for a long-term fix. If strapping helps your biomechanical function and relieves pain as well, it means that you are a candidate for a successful long-term biomechanical fix with a functional orthotic.
Functional orthotics (not arch supports or off-the-shelf “custom orthotics”) are prescribed for long-term biomechanical alignment correction, to help your feet function more effectively and make recurrence far less likely.
Conclusion
Plantar fasciitis is a very common condition. Treated early and correctly, you can be free from pain and frequent recurrence. Self-treatment can be very effective if you go at it with commitment and diligence.
If self-treatment does not significantly decrease your pain in 2 weeks, it isn’t likely to, even with more diligent self-care.
In those cases, it’s time to seek care from a pro who is a specialist in treating plantar fasciitis.
What’s been your experience with plantar fasciitis?