Your heel is designed to absorb the impact of your body weight when walking, running or doing any other form of physical exertion or weight bearing exercise.
During a typical day, your feet endure a cumulative force of several hundred tons. So it should be no surprise that heel pain is common.
In about 80% of all heel pain cases, Plantar Fasciitis (in its acute form) or Fasciosis (in its chronic form) is the underlying cause.
However, there are other injuries to your foot that have similar symptoms but aren’t plantar fasciitis, and can sometimes be made worse by incorrectly diagnosing and treating it as plantar fasciitis.
In This Article:
Heel Pain is Not Always Plantar Fasciitis
Heel pain can be caused by inflammatory joint conditions, injury, irritation and even lower back problems (conversely, untreated chronic plantar fasciitis can cause knee and back problems), so not all heel pain is plantar fasciitis.
Some of these heel related problems mimic the pain caused by plantar fasciitis.
How Can I Tell What I Have?
First, a disclaimer.
Most doctors, including me, don’t advocate self-diagnosis. The problem with self-diagnosis is, in the cases where self-diagnosis can go sideways, it can sometimes do so in a really bad way.
Self-diagnosing and self-treating foot problems seems easy, and some treatments appear simple and obvious. It’s sometimes true: it doesn’t take a rocket scientist to apply rest, ice, and elevation to help alleviate the pain from your condition.
So it appears equally simple to perform other self-treatments. Sometimes it’s a good idea. Sometimes it can make matters worse. Of course, the trick is to be able to tell the difference. It’s all in the diagnosis, and diagnosis is not as easy as it might look.
It’s not your fault; how would you know? Medical information that doctors are privy to isn’t readily found online.
Plantar fasciitis self-diagnosis is a really good example. 80% of heel pain is plantar fasciitis. People self-diagnose and treat all the time.
If you self-diagnose correctly and self-treat diligently, it’s all good. But if you get it wrong for the 20% of the time that heel pain isn’t plantar fasciitis, or self-treat inappropriately, or for too long without result, you will certainly extend your suffering, and in some cases, can pose a danger to your long term health and activity.
Chronic plantar fasciitis is much harder to treat, takes longer and can have significant biomechanical effects on your knees, back and even your neck.
Why I Wrote This Post
Proper medical care is so close and available these days, it hardly seems worth the extended pain and hard work required in self-diagnosis and care, just to avoid seeing a doctor about it and not wasting any more of your already precious time.
With that said, I know many people wind up “self-diagnosing” anyway, usually in the course of becoming educated with the good intention of having an informed conversation with a doctor.
It’s almost impossible not to, what with thousands of search results at your fingertips in milliseconds.
So, I wrote this post in an effort to save you some time, provide some guidance, and give you a frame of reference based in sound, general, medical practice.
And of course, if I haven’t droned on enough, none of this information should be construed as medical advice. These are very general observations, not to be used as a medical diagnosis or treatment recommendation of any kind. Use of this information is at your own risk.
Is Heel Pain Serious?
To the degree that you will suffer from pain and loss of function for some period of time, how serious it is can be mainly subjective; how much you need to be on your feet, how long you’ve had pain, what’s causing it, and how pain might affect you indirectly (increasingly physical and emotional stress).
Objectively speaking, long term biomechanical changes, limited functionality, and even threat of clot or embolism can be concerns, so in that regard, heel pain can certainly be serious.
For example, plantar fasciitis is a common condition, acutely not terribly serious, and in many cases will diminish and heal following a dedicated routine of self-care measures.
Other sources of heel pain may also respond well to self-care (again, done correctly, with commitment), like mild Achilles tendonitis, heel pad inflammation and pump bump.
However, if heel pain that can respond to self-care persists longer than 2-3 weeks, seek professional advice from someone who specializes in heel pain, such as a podiatrist.
Waiting longer, even with plantar fasciitis, can cause chronic problems and may put you at unnecessary risk. So, chronic plantar fasciitis can be serious.
Some heel pain problems, like Achilles tendon rupture, stress or other fractures, and tarsal tunnel syndrome, should never be self-treated. You should see a podiatrist immediately.
Here are some common causes of heel pain other than plantar fasciitis, how to spot them, and what you can do about them. Some of the data below was extracted from an article by the College of Podiatry and updated here with the latest research.
Heel Pain Causes Other than Plantar Fasciitis
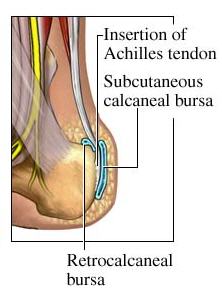
Heel Bursitis
Heel bursitis is an inflammation of a “bursa” (a fluid filled fibrous sac) on the heel bone. There are 2 bursa at the heel that can cause pain:
- the Retrocalcaneal Bursa
- the Subcutaneous Calcaneal Bursa, also called the Retroachilles Bursa
Pain is usually noticed just above the heel, and significantly worsens during the day. It may feel achy, and pressure on the back of your heel (like from shoes) can cause pain.
Sometimes the pain is made worse by flexing your foot, because it squeezes the swollen bursa.
If you have retrocalcaneal bursitis it might be painful to stand on tip-toe.
Heel bursitis is sometimes confused with Achilles tendonitis because they have similar symptoms. The Achilles tendon inserts between the 2 bursa and connects the back of the heel to the calf muscle. It can be hard to tell whether the injury is to the tendon or the bursa.
What Causes Retrocalcaneal Bursitis?
Retrocalcaneal Bursitis can be caused by
- a fall from a height onto your heel,
- overuse from walking, running, or jumping,
- a quick increase in physical activity,
- not warming up properly before exercising,
- exercising in poor-fitting shoes,
- walking in high heels.
Running uphill causes your foot to flex more than usual and can increase irritation to your retrocalcaneal bursa.
In some cases, arthritis can cause retrocalcaneal bursitis, as can damage to the Achilles tendon, osteoarthritis, rheumatoid arthritis, gout, and pseudo-gout.
What Causes Retroachilles Bursitis?
Retroachilles Bursitis is almost exclusively associated with shoes that dig into the back of your heel. It is also more likely to cause the skin at the back of your heel to turn red than retrocalcaneal bursitis.
Retroachilles and retrocalcaneal bursitis can occur at the same time, which can make the pain and inflammation more difficult to treat.
Do I Have Heel Bursitis?
With bursitis, you’ll feel pain at the back of your heel when the ankle joint is moved. There may be a swelling on both sides of the Achilles tendon at the heel. Or you may feel pain deep inside the heel when it makes contact with the ground.
Heel Bursitis (calcaneal bursitis) Treatment
Attention to the cause of any rubbing and appropriate padding and strapping will allow inflammation to settle.
Medication and ultrasound can give relief but for the long-term, a functional orthoticmay be necessary.
In Achilles tendonosis, scar tissue builds up at the site of the injury, and over time, the body begins to give-up healing the damaged tendon.
Because inflammation is not present in tendonosis, anti-inflammatory medications will not treat the condition, though it can ease discomfort.
Tendon micro-tears from everyday activities like walking or climbing stairs, and Achilles and/or calf tightness, can contribute to tendonosis, especially in the elderly.
Heel Bump (aka Pump Bump, Haglund’s Deformity)

This is a firm, painful bump on the back of the heel.
It’s called a “pump bump” because the condition often occurs due to the dress shoe heels that many women wear.
The rigid backs of the shoes create pressure that irritates that area of the heel, and women who wear pumps are the most common sufferers of this condition.
Do I Have Heel Bump?
If you have Heel Bump, you’ll see it, and it will likely be irritated and painful.
Heel Bump Treatment
Adjustments to footwear is usually enough to be comfortable. A supportive heel counter in your shoe can help.
In more serious, recurring cases, surgery may be necessary.
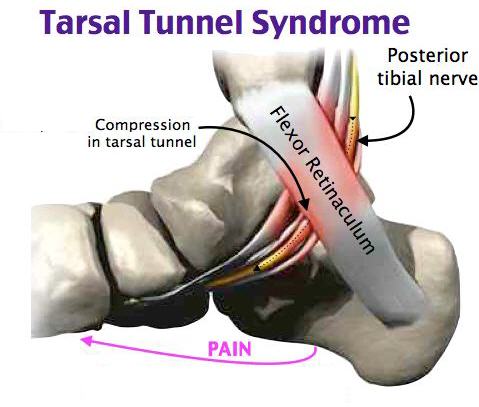
Tarsal Tunnel Syndrome
This can feel like a burning or tingling sensation in the heel area and within the arch of the foot, with occasional loss of sensation on the bottom of the foot.
This is caused by compression of the tibial nerve as it passes the inside of the ankle.
Tarsal tunnel syndrome can result from any condition that puts compression on the posterior tibial nerve, including
- flat feet or fallen arches,
- overuse,
- prolonged standing,
- excessive walking or exercising,
- swollen tendon, ganglion cyst, varicose vein,
- sprain or fracture,
- rheumatoid arthritis,
- diabetes.
Symptoms associated with tarsal tunnel syndrome include:
- pain, especially shooting pain,
- numbness,
- tingling, burning or “electric shock” sensation in the heel
- burning pain,
- shooting pain,
- sharp pain,
It can cause heel pain, ankle pain, bottom of the foot pain and even toe pain.
Patients often complain of excruciating heel pain, and sometimes incorrectly self-diagnose this problem as plantar fasciitis.
“Tinel’s Sign” is one test doctors use to help confirm a diagnosis of tarsal tunnel syndrome.
It’s positive when lightly tapping over the nerve gives you a sensation of tingling or ‘pins and needles’ along the distribution of the nerve (the paths it takes until it ends).
The distribution of the tibial nerves can cause pain in numerous areas of the foot.
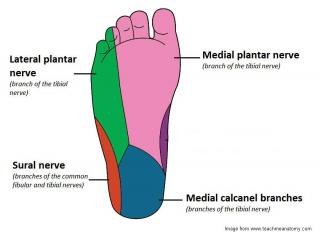
Irritated tibial nerves can cause pain in numerous areas of your foot. Some mimic severe plantar fasciitis, though are not treated the same way.
Tarsal Tunnel Syndrome Treatment
Self-treatment for tarsal tunnel syndrome is not recommended. If you are determined to try, do this for 2 weeks, and if you aren’t 100% better, come see me:
- Take an anti-inflammatory if you can
- Wear a stable shoe that prevents the heel from rolling in
- Wear an arch support in your shoes (not an expensive one, just a solid, not gel-like one)
- Don’t go barefoot at all, even in the house.
Medical Treatment for Tarsal Tunnel Syndrome
Prescription, functional orthotics can reduce the pressures on the nerve and may be appropriate for certain foot types (not all).
Sometimes local injections of medication to the area where the Tibial nerve is inflamed may be necessary.
Surgery is a last resort.
Heel Pad Inflammation
You may feel a dull ache in your heel that increases throughout the day. Pressing on the bottom of your heel may trigger pain. People sometimes mistake heel pad inflammation for plantar fasciitis.
Heel pad inflammation can be caused by
- a fall from a height onto your heel,
- chronically excessive heel strikes with poor foot gear,
- a reduction in the thickness of the heel pad.
Heel fat pad elasticity reduces with age and being overweight.
Heel Pad Inflammation Treatment
R.I.C.E. rules here. Rest Ice Compression Elevation helps when the injury is new.
Take anti inflammatory medication if you can.
It is very important to rest until there is no more pain. Continued walking or running can damage your fat pad beyond simple repair. If this happens, heel pad inflammation becomes very difficult to treat.
If you must be on your feet, use a shock absorbing and cushioning heel pad in your shoes. Wear heel pads in both shoes to maintain equal leg length.
I would also suggest taping your heel for additional protection, but this should be done in a doctor’s office.