This is the last part of this 3 part series about heel pain symptoms that can be mistaken for plantar fasciitis, but are actually due to other causes.
In this final post in the series, I’ll show you a few common conditions involving tendons that have heel pain similar to plantar fasciitis as a symptom.
I’ll also give you a few tips to prevent heel pain in the first place, and wrap up with some final comments.
In This Article:
Common Causes of Heel Pain Other than Plantar Fasciitis, Part 3
Stress Fractures
>Most stress fractures happen to active people. Falls from a height or landing on an uneven surface can cause a stress fracture, but so can chronic overuse/abuse.
Stress Fracture Symptoms
Symptoms include:
- pain that develops gradually, then becomes severe even during normal daily activities,
- pain when you put weight on the injured foot,
- pain that goes away after resting,
- tenderness to the touch,
- bruising (doesn’t always happen),
- swelling on the top of the foot or outside of the ankle. This is pretty common.
You should be able to wiggle your toes and move your foot and ankle around. If you can’t, it’s probably not a stress fracture, but something more serious.
Stress Fracture Treatment
A caution about stress fractures:
Symptoms can diminish pretty quickly once a stress fracture starts to heal. Because it doesn’t hurt as much, people sometimes resume normal activities too soon. This can delay healing further, and can actually worsen the problem. The bone may break completely.
If you notice the symptoms of a stress fracture right after an injury, follow the RICE protocol (rest, ice, compression, and elevation):
- Rest. Go non-weight-bearing. Sorry, but it’s the fastest, safest road to healing. Use crutches. If you have to bear weight for any reason, make sure you are wearing a very supportive shoe, and only for a very short while.
- Ice. Apply ice immediately after the injury to keep swelling down. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly on your skin.
- Compression. Lightly wrap the area in a soft bandage, but please ensure it is loose enough that it doesn’t cut off any circulation.
- Elevation. Rest with your foot raised up higher than your heart.
If you can, use NSAIDs (Aleve, Advil) to relieve pain and help reduce swelling.
Stress fractures need plenty of time and rest to heal; 6-8 weeks is typical, as long as you follow doctor’s orders and don’t do anything that stresses your foot and leg. Some stress fractures are harder to heal, and take longer, than others. Stress fractures to the 5th metatarsal (the long bone behind your little toe) for example, takes longer than other stress fractures.
Stress fractures of the navicular or talus may also take longer to heal.
I know it’s difficult for you runners out there. It’s tough to not run, under any circumstances, especially in our beautiful area.
I will do everything I can to make sure you can return to running, or whatever physicial activity you pursue, as soon as possible. Sometimes it just takes patience and giving your body the time to do what it needs to.
Don’t mess around if you have symptoms of a stress fracture. Come see me.
Achilles Tendonitis
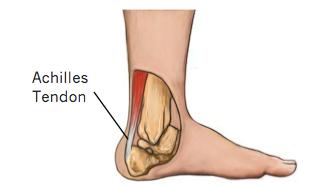
The Achilles tendon is a strong fibrous cord that connects the muscles in the back of your calf to your heel bone.
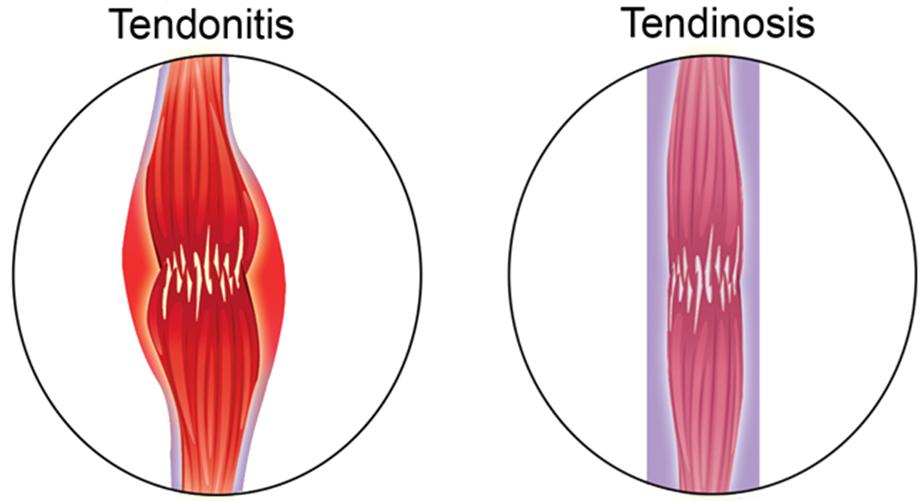
Achilles tendonitis is an acute injury to your Achilles tendon, with inflammation.
Achilles tendonosis doesn’t have inflammation, and so is treated differently.
Treating tendonosis like it’s tendonitis is futile.
Achilles tendonitis is an acute inflammation of the Achilles tendon. It’s most often caused by overuse in the course of work, athletics, or daily activities. In sports, it’s associated with repetitive movement, like golf, tennis, basketball, and running.
A direct injury can also cause tendonitis, as can inflammatory disorders, like rheumatoid arthritis.
Tendonitis is more commonly seen in people over 40 with the risk and severity of symptoms typically increasing with age.
Achilles Tendonitis Symptoms
Symptoms include
- swelling of the tendon, usually with redness, warmth and stiffness,
- tenderness directly over the tendon,
- pain with movement,
- a lump or bulge on the tendon itself.
Achilles Tendonosis
Tendonosis is a chronic, persistent, or recurring condition caused by repetitive trauma or an injury that hasn’t healed.
This condition occurs when the Achilles tendon is placed under more pressure than it can cope with, over and over. Small tears develop, and don’t heal completely.
Tendon micro-tears from everyday activities like walking or climbing stairs, and Achilles and/or calf tightness, can contribute to tendonosis, especially in the elderly.
In Achilles tendonosis, scar tissue builds up at the site of the injury, and over time, the body begins to give-up healing the damaged tendon.
Because inflammation is not present in tendonosis, anti-inflammatory medications will not treat the condition, though it can ease discomfort.
Tendon micro-tears from everyday activities like walking or climbing stairs, and Achilles and/or calf tightness, can contribute to tendonosis, especially in the elderly.
Achilles Tendon Rupture
In some cases Achilles tendonitis or tendonosis can lead to tendon rupture. Tendon rupture can be serious stuff.
Symptoms of a ruptured Achilles tendon include:
- your calf feels like its been kicked
- you have pain and swelling, possibly severe, near your heel
- you can’t bend your foot downward or “push off” the injured leg when walking
- you can’t stand on your toes on the injured leg
- you heard a “pop”, then had a sharp pain in the back of your ankle. Then you couldn’t walk.
If you have any of these symptoms, come see me right away (tell our receptionist you think you ruptured your Achilles tendon), or go to Urgent Care or the ER.
Do I Have Achilles Tendonitis or Tendonosis?
Achilles tendonitis has a similar feeling to bursitis. If you do a “pinch test” above your heel on either side of the Achilles tendon, it will be painful. You might notice some swelling.
A common symptom of Achilles tendonitis is crepitus. Crepitus is a grinding sensation that can be felt by placing your hand over a moving tendon.
Achilles tendonosis isn’t as easy to spot, because there’s no inflammation.
You may have one or more of these symptoms, if you have Achilles tendonosis:
- pain and/or tightness in the tendon behind the ankle.
- difficulty climbing stairs or running.
- pain after sitting for long periods or after sleeping.
- a bump either in the tendon (called “mid-substance Achilles tendonosis”) or right behind the heel bone (called “insertional Achilles tendonosis”).
Achilles Tendonitis Treatment
Achilles tendonitis treatment should be started as soon as possible to prevent it from getting worse.
Your main goal in tendonitis is to reduce inflammation and irritation to the tendon, and give it time to heal properly.
Unfortunately, recovery in a severe injury (or delaying treatment for too long) tends to be slow. It can take 3 to 6 months of consistent treatment to fully heal in those circumstances.
On the other hand, prompt, appropriate care can get you back to light activity in a matter of 3-4 weeks.
Rest
I know it’s tempting to “run through the pain”. The sooner you actually start treating Achilles tendonitis, the faster you can get back to playing.
The most important part of Achilles tendonitis treatment is to rest your tendon. Try to avoid activities which make your symptoms worse.
In severe cases, you might need crutches for a few weeks.
OTC Medication
Non-steroidal anti-inflammatories such as Advil and Aleve can help reduce pain, but will not reduce any thickening in the tendon caused by degeneration.
Orthotics
Wearing heel pads in your shoes during the early acute stage of inflammation can reduce tension on the tendon. Find something inexpensive.
It is also important to find out if your tendonitis has any altered foot biomechanical component. This is best done by a podiatrist who specializes in heel pain.
Although you may be tempted to self-treat with rest, ice and elevation to avoid a trip to my office (no offense taken), taking a look at your biomechanical alignment, and fixing anything misaligned there, will go a long way to preventing painful recurrence.
Low Impact Exercise
Switching to activities such as swimming and cycling (please get physician OK first) put much less strain on the Achilles tendon than high impact activities like running.
If you give it time and don’t strain the tendon, you should ultimately be able to return to your sport of choice at 100%.
Stretches
Don’t start to stretch your Achilles tendon or calf muscles until you can raise up onto your tiptoes pain-free.
At that point, light calf stretches, heel raises and drops will help get that tendon back in shape. Go easy. Listen to your body.
Physician Care of Achilles Tendonosis
In addition to the self-care I mention above, I recommend the following additions:
- Physical therapy to break down scar tissue and increase blood supply
- Functional orthotics to correct foot misalignment
- Bracing or walking boot to protect the tendon as needed
- Extracorporeal shock wave therapy (ESWT) as needed.
Rupture Treatment
In general, for complete tear of the tendon, surgery is the usual solution.
For partial tears, I recommend non-surgical care depending on your age, activity level and other risk factors.
How Do I Prevent Heel Pain?
In general, prevention for many of these problems is similar:
- Avoid wearing ill-fitting or uncomfortable shoes
- Wear shoes with good heel cushioning and effective arch support (you may need a functional orthotic)
- Avoid walking or exercising on hard ground
- Rest regularly and try not to walk or run too fast if you already have heel pain
- Wear a slight raised heel (1/2″ or so)
- Lose weight if you are overweight
Conclusion
Heel pain can have many causes other than plantar fasciitis, but the symptoms can be almost exactly the same.
You can certainly try self-treatment; the risk is treating without a proper diagnosis.
I truly admire your commitment to good health and self-treatment. I’m always happy to help you sort out what’s going on, and give you a plan that fits with your lifestyle.
Your loved ones and community deserve the best “you” you can give, so struggling with a mystery foot problem may not help them.
And they worry about you, too.