Today, I’m going to give you a few simple tips to help you find a physician who has the chops to really cure your plantar fasciitis.
In This Article:
Not All Doctors Know What They’re Doing with Heel Pain
Shocking, isn’t it? Not that some doctors don’t know how to treat a particular problem (we all know that, right?), but that another doctor will admit it.
I’ve no doubt some physician is going to read this and lambast me for having the thought, much less putting it in writing. I won’t be winning any popularity contests anytime soon at physician conferences.
Of course a doctor doesn’t know everything. It’s impossible. Even specialists aren’t all equal when it comes to knowledge, communication, and experience. Not even close.
It’s not necessarily a flaw of the particular doctor; medicine is a very fast moving, global research-heavy field.
Endless daily demands make it difficult for physicians to stay on top of every new discovery. There isn’t a mechanism or process yet to alert them with what might be relevant to their specialty.
So it takes steadfast commitment and effort to do so, while keeping a normally hectic, demanding schedule. Not every doctor can do that, or wants to.
And, of course, within every field, as in medicine, not everyone working in it was at the top of their class. Competency naturally varies.
On the upside, some physicians specialize within a specialty, so these physicians are often very, very good at that sub-specialty (like curing heel pain).
There aren’t licenses to validate these niche experts. Physicians who sub-specialize try to structure their required continuing medical education towards their sub-specialty interest, and are known by reputation.
For patients, the trick is finding these gems when you need them.
It’s Hard to Know if a Doctor is Good at What They Do
Unfortunately, it’s almost completely impossible for patients to know if a doctor is actually really good at what the patient needs them to be really good at. Frankly, physicians sometimes have the same problem when handling their own care.
How do we usually find a doctor?
We ask people we trust. We get another physician’s recommendation. We use reviews, though we know not to blindly trust them. We figure if the guy has mainly good reviews, he must be OK. Not true, of course, but it’s one of the very few resources we have to make some kind of informed decision.
Sometimes we go because the office is close by.
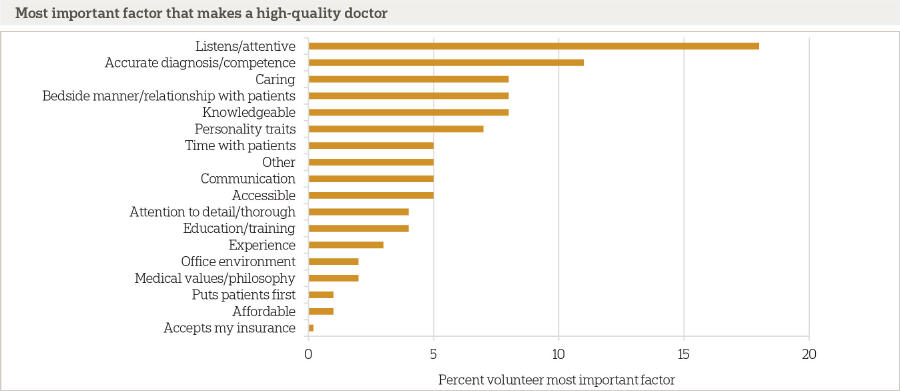
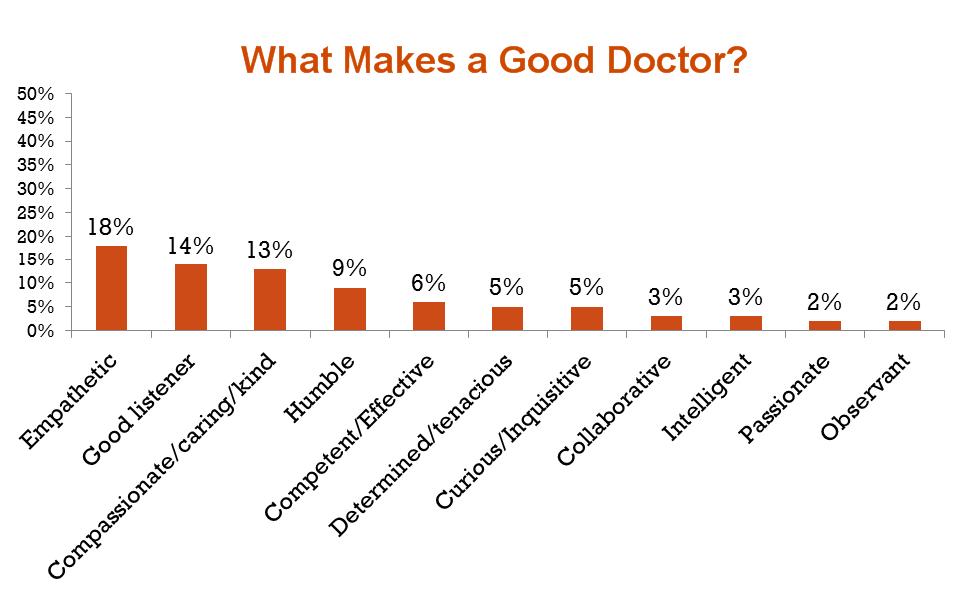
A comprehensive, recent study from the Associated Press-NORC Center for Public Affairs Research shows what most people consider important when choosing a physician.
When asked to describe a “high-quality” provider, most Americans focus on the doctor-patient relationship. By far, that a physician listens and is attentive is the most important quality they must demonstrate.
A key finding about the quality of a doctor was not surprising:
Certainly not a patient’s fault. The study indicated it was very difficult for patients to find and evaluate information that might give them an objective assessment of a physician’s quality.
An informal Twitter poll recently done by a physician showed that most people assume physicians meet a threshold of intelligence, knowledge, and judgment. Therefore, what differentiates good doctors from mediocre ones is the “soft stuff” like empathy, listening; you know, those things that show the guy cares enough about you to make a sincere effort to properly treat you.
Because doctors all meet some threshold of competence evidenced by board certification and licensure, we often assume they know what they’re doing.
As we all know, it isn’t always true.
The wide variation in capability and clinical judgment among medical practitioners I see actually prompted this blog post. I think we need to do a bit better than just a soft assessment where we can.
When to Look for a Great Plantar Fasciitis Specialist
Plantar fasciitis is one of the most common, most incredibly painful conditions people can get. And when you have it, you need fast, effective care.
Most people (65%) try self-treatment first, often for 6 months or more.
It’s not a great idea (I’ll tell you why in a moment), but it’s certainly understandable:
- People are busy; going to a doctor takes time.
- They “tough it out” (some of us were just raised that way).
- Sometimes they worry about what “it” might really be (“OMG, maybe I have cancer!”) and don’t really want to know.
I get it.
Here’s the problem:
The longer you have untreated plantar fasciitis, the less likely you will improve from conservative treatment, even from a doctor.
Why?
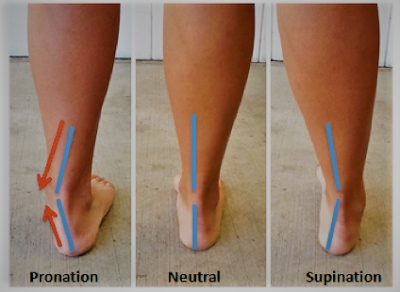
Because the condition is ultimately caused by a biomechanical misalignment that traumatizes your plantar fascia. This causes your body to create scar tissue and further alter its alignment in an effort to heal and compensate.
Over time, increasing misalignment creates more trauma to the plantar fascia. And so the cycle continues until your pain, and the reason for it,becomes a monster.
Treatment then becomes much harder, more costly, and takes longer. You may not respond to conservative care well, if at all.
This altered alignment can also harm your knees, back, and even your neck.
So waiting too long to do something effective about your plantar fasciitis is not your best option.
How long to wait?
If you’ve had heel pain for a month or 2 without having done any self-care, come see me. Things will become chronic soon.
If you’ve been self-treeating for more than 2 weeks without a significant reduction in pain, it’s also time to see me.
Acute plantar fasciitis can be resolved without surgery 98% of the time. So don’t wait too long to resolve yours.
When it’s time to get professional help, give me a call.
Narrowing the Field: Who Can Treat Plantar Fasciitis?
Here are the typical players who see patients with plantar fasciitis:
Primary Care / Family Physician:
Your primary care physician is not specially trained to treat plantar fasciitis but may be able to offer some initial self-treatment activities. They may or may not know of a competent heel pain specialist.
Your insurance company might require a pre-authorization from a primary care physician to see any specialist, so check before making an appointment with one.
Orthopedist/Orthopedic Surgeon:
Orthopedists are doctors who concentrate on surgically correcting deformities in, or functional problems with, your bones and associated muscles and ligaments.
They often specialize in certain parts of the body: spine, shoulders, hands, hips, knees, foot and ankle, etc.
If you want to see an orthopedist, make sure they specialize in foot and ankle, and have a mindset that approaches your plantar fasciitis conservatively, with surgery as a last resort.
Podiatrist:
A podiatrist is to the foot what a dentist is to teeth, or an ophthalmologist to the eye. They specialize in the prevention, diagnosis and treatment of foot disorders resulting from injury or disease.
Statistically, podiatrists treat the majority of people with plantar fasciitis that requires physician care.
Podiatrists can do everything an orthopedic foot surgeon can do, as well as resolve non-surgical dermatological and biomechanical problems of the foot and ankle.
A podiatrist is more likely to treat your pain or discomfort using a conservative approach, with surgery as a very last resort.
However, not all podiatrists sub-specialize in biomechanics, sports medicine, or difficult plantar fasciitis cases.
Physical Therapists:
Podiatrists work with physical therapists to help resolve stubborn plantar fasciitis cases, and can be very helpful in this regard.
Because physical therapists do have a limit as to the scope they can diagnose and treat, it’s wise to have a physician determine whether your heel pain is actually plantar fasciitis before seeing a physical therapist for exercises and therapy to resolve it.
Orthotists and Pedorthists
Orthotists and Pedorthists don’t actually treat medical conditions.
They design, fabricate, assemble, fit, and adjust or modify foot orthotics, custom footwear, and some ankle and foot braces. They aren’t doctors, but work with doctors who give them a prescription to make an orthotic or brace for your foot and condition.
How to Find the Best Plantar Fasciitis Treatment Specialist for You
When self-treatment fails, you need help from a competent physician.
Having some objective way to gauge a physician’s competency to quickly, accurately and effectively treat your plantar fasciitis can make the difference between a not-so-good experience and a really great one.
Here’s how to know if you’ve found a competent physician who can treat your plantar fasciitis.
The 2 Key Questions to Ask Before You Make an Appointment
Getting answers to 2 key questions will go a long way to helping you find a physician who really knows what they’re doing with plantar fasciitis.
Why These 2 Key Questions?
These 2 questions:
- give you a real, medically valid edge to finding the right level of expertise needed to make sure your condition resolves quickly
- ensure you don’t need to be a medical expert to know if the answers are appropriate
- let the physician’s office know you’ve done some homework and expect excellent care
You’ll soon see that these 2 questions ask about prescription orthotics. I don’t know if you need orthotics. And the questions aren’t really about orthotics; they just seem to be.
The reason you ask these particular questions is that the way the physician approaches orthotics often indicates the general degree of expertise he has with plantar fasciitis.
Plantar fasciitis is a biomechanical problem. Proper creation of prescription orthotics requires a deep understanding of biomechanics.
So how the physician deals with the first steps of creation of an orthotic is telling as to their general expertise with the condition overall.
If they understand plantar fasciitis, they’ll know the proper way to make a mold of your foot for an orthotic that will restore proper biomechanical function of your foot, which will allow you to heal, and remove pain in the process.
Ask these questions before you make an appointment to diagnose and treat your heel pain (80% of heel pain is from plantar fasciitis):
The Key Questions
Key Question #1: “If I need prescription orthotics, will the doctor personally cast me?”
- Some doctors have medical assistants cast. Avoid this office.
- Some doctors cast personally. This is a good first answer. The next question will indicate how much they know about biomechanics and, by association, your plantar fasciitis (which is most often a biomechanical issue).
- Some doctors send you to an Orthotist or Pedorthist to cast you. Although sending to an Orthotist or Pedorthist is perfectly fine, it might be an indication of the physician’s interest and knowledge, or lack thereof. If you’ve seen other physicians without resolution, this physician choice may not be the best one to make.
Orthotists and Pedorthists work with knowledgeable physicians and could be a good source for finding a really good doctor for your chronic plantar fasciitis. So you could always call and ask them who they’d send their loved ones to, if they had plantar fasciitis pain.
If you’re going to have an Orthotist or Pedorthist cast you, ask the same 2 key questions that you’d ask of a potential physician choice.
Key Question 2: Ask this after you know that the Physician / Orthotist/ Pedorthist casts personally:
Ask: “What method do you use to cast for a prescription orthotic?”
The correct answer has 2 parts:
Correct Answer Part 1: The doctor casts you “Non-weight bearing, in neutral (position)”. This is key.
Correct Answer Part 2: They use plaster or a 3D scanner.
What does “non-weight bearing, in neutral position” mean?
Foot castings or impressions capture accurate images of your feet, which become the blueprint for your orthotic. The orthotics are then used to correct, support, align, and prevent dysfunction of (or improve the function of) your movable body parts.
The idea here is to correct the misalignment in your foot and its relation to rest of your body This reduces plantar fasciitis pain AND helps correct the reason you got plantar fasciitis.
In order to do this, your doctor needs to make sure the cast made from your foot results in the orthotic actually correcting the problem, so your foot needs to be in its “corrected” position during the casting.
This “corrected” position is usually “neutral”, meaning your foot isn’t tilted side to side or back to front. .
If your foot wasn’t placed in a neutral position, you’d just get a mold of your out-of-alignment foot. That won’t correct anything. It would likely relieve pain in the short term, but you could get that for $50 in a retail store or my office.
As a note, there is the rare occasion that your foot should be cast in something “not neutral”. For the vast majority of plantar fasciitis sufferers, casting in neutral is medically appropriate.
Along with being cast in a neutral position, you’ll also be “non-weight bearing”, or not standing (unlike in the photo above).
“Non-weight Bearing”
If you have weight on your foot when casting or making an impression to build an orthotic mold, your foot will also be in its out-of-alignment position.
The only way to get the foot in a corrected position is to
- make sure your foot is adjusted so its not out of alignment (“neutral” position), and
- not have any weight on it, (“non-weight-bearing”).
When your doctor casts you, he’ll make sure you are non-weight bearing and in neutral while he lets the plaster cast harden or takes the 3D scan.
Some doctors cast with your feet pointing down; others have you lay on your back so your toes point up. Either is OK.
What does casting using plaster or 3D scanning mean?
Plaster Casting
Literally, the doctor uses sheets of material soaked in a medical plaster. He wraps these strips in a very specific way to make a precision mold of your foot, which the Orthotist uses to manufacture your one-of-a-kind functional orthotic.
3D Orthotic Scanning
There are scanners out now that replace the need for plaster. The scanner is held up to your foot while it is in a neutral, non-weight bearing position, and creates a digital image.
The Orthotist then uses the digital 3D impression to fabricate your orthotic.
Whether the doctor casts you using plaster or a 3D scanner, it’s the doctor’s skill and understanding of foot biomechanics that makes it all work.
What if They Start Saying a Bunch of Stuff I Don’t Understand?
Here’s what to look for, that disqualifies them, if they don’t directly answer your question. They’ll tell you they cast by having you:
- walk on a flat pad or over something flat,
- stand on or in anything (a scanning pad, a foam box, a shallow pond with small alligators),
or
- they won’t tell you what method they use, and/or
- they don’t understand your question (you can clarify with the front desk or a medical assistant that you want to know if they cast non-weight bearing in neutral).
If they sound confused, it’s probably a bad sign (give them the benefit of the doubt first, and ensure you are speaking to someone with clinical knowledge of what happens in the office).
Conclusion
There’s so much “information” (some of it is just a crock) on the internet about plantar fasciitis, you’d think it was pretty easy to fix.
And for the most part, that could be true if your situation hasn’t been going on very long and you are very diligent about the stretching, icing, exercise instructions and routine commonly advised.
When the simple stuff isn’t working well and quickly, you’re in new territory.
Seeing a physician who isn’t expert in plantar fasciitis care might just wind up delaying necessary healing, or making matters worse.
I’ve seen untold numbers of online comments by people who suffer endlessly, seeking treatment from numerous physicians without relief, their condition worsening by the visit.
It gives the rest of us a bad name (painted with the same, broad brush of incompetence). It’s heartbreaking for patients and unfair to actually good doctors.
I hope to save as many of you from that agonizing physical and emotional stress as I can by telling you the truth of what’s what with plantar fasciitis.
Asking these 2 questions won’t guarantee you’ll find the perfect doctor, but they can help cull out a fair number of doctors who may not cut it for your more complicated case.
Please use them.
A Final Note:
If you’re interested in what a doctor has to know and do to properly cast for a prescription orthotic, this heady article gives a pretty good idea.